Sjögren's Center

Welcome to the Columbia Sjögren's Center, a leading facility dedicated to the comprehensive care of individuals affected by Sjögren's syndrome. Located within the renowned Columbia University Medical Center, our center brings together a multidisciplinary team of experts dedicated to the care of Sjogrens patients.
Committed to advancing the understanding and management of this complex autoimmune disease, we provide compassionate care while actively engaging in cutting-edge research to improve outcomes and quality of life for those affected by Sjögren's Disease. We are committed to providing personalized treatment plans that address both the systemic and symptomatic aspects of this complex autoimmune disorder.
Beyond patient care, the Columbia Sjögren's Center is at the forefront of research and education aimed at advancing the understanding of Sjögren's syndrome. We actively participate in clinical trials and studies to explore new therapeutic options and improve existing treatments. Our commitment to innovation and collaboration extends to educating healthcare professionals and raising public awareness about the disease. By integrating compassionate care with cutting-edge research, we strive to enhance the quality of life for our patients and contribute to global efforts to find better treatments.
What is Sjögren's Syndrome?
Sjögren's (SHOW-grins) syndrome is a chronic autoimmune disease that targets the moisture-producing glands and mucose membranes in the mouth and eyes, resulting in dry eyes and mouth. Sjögren's syndrome often accompanies other autoimmune disorders, such as rheumatoid arthritis and lupus. It is one of the most common autoimmune disorders with more than four million Americans living with the disease. Nine out of 10 patients are women. The average age for onset of this disease is late forties.
There are two types of Sjögren’s syndrome: primary and secondary. Primary Sjögren’s syndrome refers to patients with gland inflammation (resulting in dry eyes and mouth) and no other underlying rheumatologic condition. Secondary Sjögren’s syndrome refers to patients with Sjögren’s and another rheumatologic condition, such as rheumatoid arthritis, systemic lupus erythematosus (SLE or lupus), or scleroderma. The distinction is important because it informs your prognosis and how you are treated. Our world-renowned specialists have years of experience researching, developing, and providing the most effective treatments. At the Sjögren's Center we understand that as the severity and number of symptoms vary greatly, so must your care.
Our Team
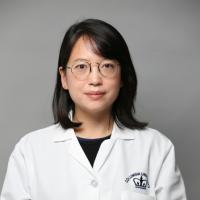
Teja Kapoor, MD
- Sjögren's Center Director | Division of Rheumatology and Clinical Immunology
Dr. Teja Kapoor is the Director of the Columbia Sjogren’s Center. She is an Assistant Professor of Medicine at Columbia University College of Physicians and Surgeons in the Division of Rheumatology.
Dr. Kapoor has clinical and research interests in Sjogren's Disease and Systemic Lupus Erythematosus (SLE), with years of experience in managing patients with complex multi-organ involvement of their autoimmune disease. She has lectured on SLE and Sjogren's Disease at regional, national, and international conferences, with a multitude of book chapters and peer-reviewed article publications on the topics of autoimmune diseases. She is a member of the national collaboration network of Sjogren’s specialists “Sjo-Net” and a member of the OMERACT Sjogren’s Working Group.
She is the Fellowship Program Director for the Columbia Rheumatology Fellowship Training Program. She is the Course Co-Director for Rheumatology and Clinical Immunology medical student course at the Columbia Vagelos College of Physicians and Surgeons. She is the recipient of the 2023-2024 Daniel V. Kimberg Memorial Junior Faculty Award for outstanding teaching of fellows, residents, and medical students. She is also on the Columbia Medicine Grand Rounds Organizing Committee and on the Education Committee of the American College of Rheumatology (ACR).

LeeJee Suh, MD
- Cornea Service | Department of Ophthalmology
Dr. Leejee H. Suh, is the Director of the Cornea Service at Columbia University's Edward S. Harkness Eye Institute and the Miranda Wong Tang Associate Professor of Ophthalmology.
She completed her Optho residency at Johns Hopkins Wilmer Eye Institute, and Cornea fellowship training at Bascom Palmer Eye Institute at the University of Miami Hospitals, where she was on faculty. Dr. Suh published numerous peer-reviewed articles and book chapters on corneal conditions and is active in clinical research. She has a clinical and research interest in Sjogren’s Disease. In addition to Sjogrens, her clinical research interests are in keratoconus research and treatments, namely Corneal Collagen Crosslinking. She has been the Principal Investigator for the Corneal Collagen Crosslinking trial for the treatment of keratoconus and post-refractive surgery ectasia at Columbia University. For her work in keratoconus, Dr. Suh has been named a Top Doctor for the National Keratoconus Foundation (NKCF) and was instrumental in the early studies of a newer type of partial corneal transplantation, called endothelial keratoplasty, both of which have dramatically changed the face of surgical treatments for corneal diseases. Dr Suh lectured nationally and internationally on her research and experience.

Elizabeth Philipone, DMD
- Oral & Maxillofacial Pathology | Department of Pathology and Cell Biology
Dr. Elizabeth Philipone is an Associate Professor of Dental Medicine (in Pathology and Cell Biology) at the Columbia University Medical Center. She is the Division Director and Residency Director for the Oral & Maxillofacial Pathology Program. Her clinical and research interests include the diagnosis and treatment oral mucosal diseases including vesiculobullous conditions, viral and fungal infections, Sjogren's syndrome and pre-cancerous/cancerous conditions of the oral cavity. She is board-certified in Oral and Maxillofacial Pathology.
![]()
Stephanie Purisch, MD
- Maternal-Fetal Medicine | Department of Obstetrics and Gynecology
Dr. Stephanie Purisch is a maternal-fetal medicine specialist and assistant professor of obstetrics and gynecology at Columbia University Irving Medical Center. She joined the Division of Maternal-Fetal Medicine at Columbia after completing residency in obstetrics and gynecology at the Hospital of the University of Pennsylvania and fellowship in maternal-fetal medicine at Columbia University.
Dr. Purisch is the co-director of the Mothers Center Heart Program, which provides comprehensive, multidisciplinary clinical care to women with cardiovascular disease who are pregnant or contemplating pregnancy.
Dr. Purisch's primary clinical and research interest is the care of women with medically complicated pregnancies. In addition to cardiac disease in pregnancy, she also has expertise caring for pregnant women with underlying maternal pulmonary, endocrine, rheumatologic, and hematologic diseases.

Stephanie Levasseur, MD
- Pediatric Cardiology | Division of Cardiology
Dr. Stephanie Levasseur is the Medical Director of Fetal Cardiology at Columbia and an Associate Professor of Pediatrics at CUMC.
Dr Levasseur joined the division of Pediatric Cardiology in 2003 after completing her cardiology training at Toronto's Hospital for Sick Children and a year of advanced echocardiography at Boston's Children's Hospital.
Dr Levasseur's passion for the prenatal diagnosis of cardiac anomalies and the support of affected families developed early in her cardiac imaging career. Her practice is dedicated to the care of the most complex patients with congenital heart disease before and after birth. The Fetal Cardiac Program at Columbia University Medical Center is one of the largest in the country. In 2012 and became director of the noninvasive imaging laboratory (which includes echocardiography, fetal cardiology as well as cardiac magnetic resonance imaging and cardiac computed tomography imaging) in 2016. She is the site PI for the STOP BLOQ study: "Surveillance and Treatment tO Prevent Fetal Atrioventricular Block Likely to Occur Quickly".

Claire McGroder, MD
- Division of Pulmonary, Allergy and Critical Care
Dr. Claire McGroder is an Assistant Professor of Medicine in the Division of Pulmonary, Allergy and Critical Care. She specializes in caring for patients with interstitial lung disease (ILD) and pulmonary fibrosis. Her clinical and translational research has focused on gaining a better understanding the earliest stages of pulmonary fibrosis. She is also studying the long-term pulmonary effects of COVID-19. Clinically, Dr. McGroder is involved in numerous clinical trials that investigate possible therapeutics for patients with ILD. It is her goal to integrate Columbia's top-tier research and excellent clinical diagnostics and resources to provide patients with the best possible care.

David Zhang, MD
- Division of Pulmonary, Allergy and Critical Care
Dr. David Zhang is a clinician-researcher with a focus on interstitial lung disease. He sees patients in the ILD clinic at Columbia University and manages patients with connective tissue disease related ILD, hypersensitivity pneumonitis, IPF, post-COVID fibrosis, among many other conditions. Additionally he is focused on conducting novel basic and translational research using next generation sequencing technology on patients with interstitial lung disease, including those with idiopathic pulmonary fibrosis (IPF).

Thomas Brannagan III, MD
- Peripheral Neurology | Division of Nephrology
Dr. Thomas Brannagan is the director of the Peripheral Neuropathy Center and co-director of the EMG laboratory at Columbia University Medical Center.
He completed his Neurology residency training at the Neurological Institute of Columbia Presbyterian Medical Center between 1991 and 1994. He subsequently did a Neuromuscular EMG fellowship at Columbia, followed by a Neuroimmunology fellowship in the laboratory of Dr. Norman Latov. Prior to returning to Columbia, Dr. Brannagan was the director of the Diabetic Neuropathy Research center at Cornell University in New York City.
He is a member of the American Academy of Neurology, the American Neurological Association, as well as the American Association of Electrodiagnostic Medicine. He is also a member of the International Society of Amyloidosis and the Peripheral Nerve Society.
He currently sees patients with peripheral neuropathies and does electrodiagnostic studies, as well as conducts clinical research and clinical trials for new treatments for peripheral neuropathy, with a special interest in Sjogren’s small fiber neuropathy, hereditary transthyretin amyloid polyneuropathy and chronic inflammatory demyelinating polyneuropathy (CIDP).

Sarah Wesley, MD MPH
- CNS Neuro-Immunologist
Dr. Sarah Flanagan Wesley graduated from medical school at the Royal College of Surgeons in Dublin, followed by residency in adult neurology at the Icahn
School of Medicine at Mount Sinai and then fellowship in neuroimmunology at the Yale School of Medicine. Dr. Wesley was on faculty at Yale as an Assistant Professor of Neurology in the neuroimmunology subdivision until joining faculty at Columbia in 2020.
Dr. Wesley treats a range of neuroimmunological and autoimmune neurological conditions, including various forms of autoimmune encephalitis, CNS vasculitis, neuro-rheumatological conditions, multiple sclerosis, and immune-related toxicity to cancer treatments.
Dr. Wesley serves as a lead for Columbia's neurological immunotoxicity program, conducting clinical and translational research on the mechanisms and management of neurological side effects to cancer treatments, such as cancer immune checkpoint inhibitors and CAR T-cell therapy.

Louis Weimer, MD
- Neurology-Autonomic Dysfunction | Division of Neurology
Dr. Louis Weimer directs the EMG laboratory and the Clinical autonomic laboratory and co-directs the Columbia Neuropathy Research Center.
His clinical and research interests include autonomic and small nerve fiber function, dysautonomia, peripheral neuropathy, neurologic causes of syncope, and autonomic failure syndromes.
Former board of director member of the American Association of Neuromuscular and Electrodiagnostic Medicine. He is a counsel member of the UCNS accreditation board. He is the chair of the quality assurance committee for the department of neurology.
He has written numerous papers, book chapters, and review articles and reviews papers for several medical journals and is a section editor for Medlink Neurology and Current Neurology and Neuroscience Reports.
In addition to patient testing, Dr. Weimer sees patients in consultation, in most instances patients with various forms of autonomic dysfunction, peripheral neuropathy, and neuromuscular disorders.

Yiming Luo, MD
- Rheumatology Genetics | Division of Rheumatology and Clinical Immunology
Dr. Yiming Luo has a keen interest in the full spectrum of complex immune-mediated rheumatic diseases, including those with diagnostic uncertainty.
Dr. Luo leads a multidisciplinary rheumatology genetics clinic, aiming to provide molecular diagnoses for patients suspected of having rare monogenic immune disorders, some of whom may present as Sjogren's-like diseases.
Dr. Luo completed his rheumatology fellowship at the National Institutes of Health (NIH), where he also received a Master of Health Sciences degree through the NIH-Duke Clinical Research Training Program. Dr. Luo has received the Scientist Development Award from the Rheumatology Research Foundation. Dr. Luo's ongoing research focuses on elucidating the genetic underpinnings of complex autoimmune rheumatic diseases.
He works alongside Joshua Milner, MD is a leader in the field of discovery and immunopathogenesis of genetic diseases. Dr. Milner was chief of NIH’s Allergy and Infectious Disease institute (NIAD).

Elizabeth Park, MD, MPH
- AI Bioinformatics & Large Data Sets | Division of Rheumatology and Clinical Immunology
Dr. Elizabeth Park is an Assistant Professor of Medicine at Columbia University Vagelos College of Physicians and Surgeons in the division of Rheumatology.
She has completed a master’s degree focusing on biostatistics, data science, and bioinformatics through the Mailman School of Public Health.
She utilizes AI and the electronic health record (EHR) to generate large, observational cohorts and has received training grants from the NIH, Rheumatology Research Foundation, and Pfizer. She also works with graduate students from the Data Science Institute at Columbia University on clinical informatics projects.

Our Location
Make An Appointment
ColumbiaDoctors Rheumatology & Clinical Immunology is a leader in the care and treatment of rheumatic disease, offering the latest therapies for patients of all ages. Many of our treatment services are also offered through participation in research studies.
To make an appointment or referral with a member of our Sjögren's Care team, please call 212-305-4308 and our office will schedule your appointment.
Connect Patient Portal
Current patients can count on secure messaging, the use of our online bill payment feature, and 24/7/365 access to their healthcare information through the Connect online portal.
Signing up for Connect is easy. Ask about joining Connect at your next visit. If you already have an invitation and activation code, visit our sign-up page. If you do not have an activation code, visit our self-sign-up page and follow the directions.
Connect is a joint effort of Columbia, NewYork-Presbyterian, and Weill Cornell Medicine, so a single Connect account links you to all three institutions.